Understanding the HPV Virus
The hpv virus, also known as human papillomavirus, is one of the most common infections out there, affecting millions of people worldwide every year. It’s a sneaky little thing that often goes unnoticed, but here’s the good news: in most cases, your body fights it off without any fuss. As we dive into this topic, we’ll explore what makes the hpv virus tick, how it spreads, and why staying informed can make all the difference. Think of it as arming yourself with knowledge – after all, prevention is better than cure, right?
This virus isn’t something rare or exotic; it’s practically everywhere. Experts estimate that nearly everyone will encounter the hpv virus at some point in their lives, but the vast majority won’t even know it. That’s because many infections clear up on their own, leaving no trace behind. However, understanding the hpv virus helps us appreciate the steps we can take to protect ourselves and others. Let’s break it down step by step, starting with the basics.
What Exactly is the HPV Virus?
At its core, the hpv virus is a group of more than 200 related viruses that infect the skin and mucous membranes – those moist linings in places like the mouth, throat, and genitals. These viruses are tiny, non-enveloped DNA particles that target epithelial cells, which are the cells on the surface of your skin and inside your body. They’re so small you can’t see them without a microscope, but they’ve been around for ages, evolving alongside humans.
What sets the hpv virus apart is its ability to cause cellular changes. Some types lead to harmless growths, while others can be more serious. But don’t worry – the body’s immune system is pretty amazing at handling most infections. In fact, about 90% of hpv virus infections resolve spontaneously within two years, without any treatment needed. That’s a testament to how resilient we are. However, persistent infections from certain strains can linger, and that’s where awareness comes in handy.
Interestingly, the hpv virus is species-specific, meaning it only affects humans – no need to blame your pets! It’s part of the Papillomaviridae family, and scientists have been studying it for decades, leading to breakthroughs like vaccines. If you’ve ever wondered why warts pop up on hands or feet, that’s often a low-risk hpv virus at work. But when it comes to genital areas, things can get a bit more complex, yet manageable with the right info.
This illustration gives a glimpse into the structure of the hpv virus, showing its capsid proteins that help it attach to cells. Seeing it like this reminds us it’s just a virus, not invincible.
How the HPV Virus Spreads
Spreading like wildfire in close contact situations, the hpv virus primarily transmits through intimate skin-to-skin contact. That often means during sexual activity – vaginal, anal, or oral – but hey, it’s not limited to that. Even without full intercourse, if there’s genital touching, the virus can hitch a ride. And get this: you can pass it on even if you don’t have visible symptoms, which is why it’s so widespread.
But let’s keep things optimistic – knowing how it spreads empowers us to prevent it. For instance, using condoms reduces the risk, though not entirely, since the virus can affect areas not covered by them. Mothers can also pass the hpv virus to babies during childbirth, but that’s rare and usually harmless. Sharing personal items like razors isn’t a common way, as the virus prefers warm, moist environments.
In everyday life, non-genital hpv virus types spread through cuts or abrasions on the skin, like when kids get warts from playing around. Transitional phrases aside, the key takeaway is that education turns the tide. By talking openly about the hpv virus, we reduce stigma and encourage safer practices. After all, it’s not about fear; it’s about smart choices that keep us healthy.
Common Symptoms Associated with HPV Virus
Oh boy, symptoms of the hpv virus can be tricky because often, there are none at all – it’s like a silent visitor that comes and goes. When they do show up, they’re usually benign, such as warts on the skin or genital areas. These warts might look like small, flesh-colored bumps or clusters, sometimes resembling cauliflower. They can itch or cause discomfort, but they’re treatable.
For high-risk types, symptoms might not appear until years later, manifesting as abnormal cell changes detected through screenings like Pap smears. Women might notice unusual vaginal discharge or bleeding, but again, early detection is a game-changer. Men could experience warts on the penis or around the anus, yet many remain asymptomatic.
The bright side? Most people clear the hpv virus without ever knowing they had it. If symptoms arise, doctors have plenty of options to manage them, from creams to minor procedures. Interjections like “thank goodness” fit here because advancements in medicine make dealing with symptoms straightforward. Remember, noticing something unusual? Get checked – it’s always better safe than sorry.
Different Types of HPV Virus
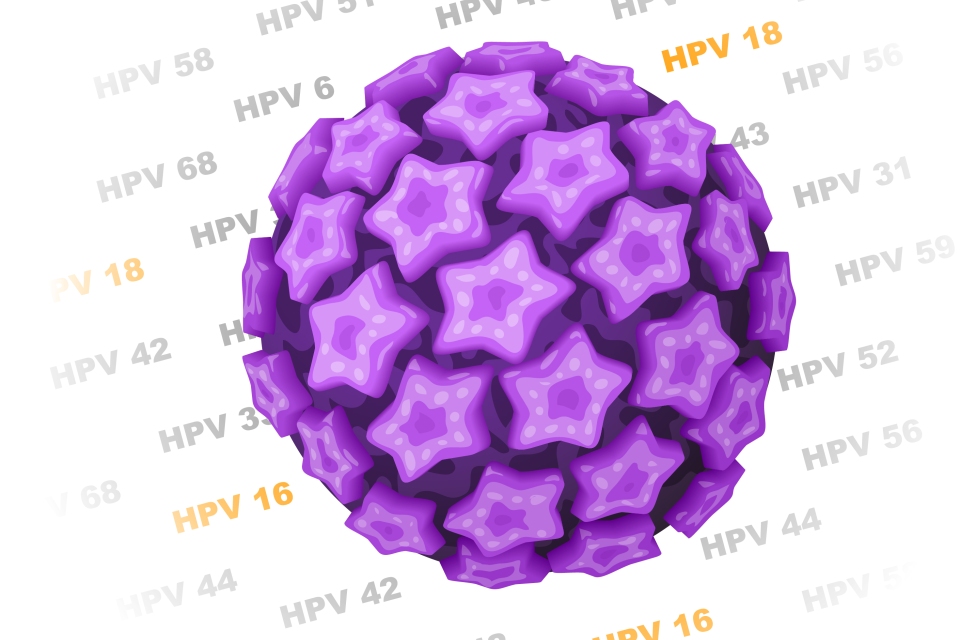
Diving deeper, the hpv virus comes in a staggering variety – over 200 types, each with its own number, like HPV-16 or HPV-18. They’re broadly categorized into low-risk and high-risk groups. Low-risk ones, such as HPV-6 and HPV-11, typically cause warts but rarely lead to cancer. High-risk types, including HPV-16 and HPV-18, are the ones to watch, as they account for about 70% of cervical cancers.
Here’s a quick breakdown in a table to make it clearer:
| Type Category | Examples | Common Effects | Risk Level |
|---|---|---|---|
| Low-Risk | HPV-6, HPV-11 | Genital warts, skin warts | Low – Mostly harmless, clear up on own |
| High-Risk | HPV-16, HPV-18, HPV-31 | Potential for cell changes leading to cancer | Higher – But preventable with vaccines and screenings |
| Other | HPV-1, HPV-2 | Common warts on hands/feet | Very low – Non-sexual transmission |
This variety shows why the hpv virus is so ubiquitous, but also why targeted prevention works wonders. Some types infect specific areas, like the mouth or throat, leading to conditions like oral warts. Yet, with vaccines covering the most dangerous ones, we’re in a better position than ever to tackle the hpv virus head-on.
The Link Between HPV Virus and Cancer
Now, let’s address the elephant in the room: the connection between the hpv virus and cancer. Not all types cause cancer – in fact, most don’t. But persistent infections from high-risk strains can lead to cellular changes over time, potentially resulting in cancers of the cervix, anus, penis, vulva, vagina, or oropharynx (back of the throat). Cervical cancer is the most common, but even there, it’s often preventable.
The process isn’t overnight; it can take years or decades for abnormal cells to turn cancerous. That’s why regular screenings, like Pap tests or HPV tests, are lifesavers – they catch issues early when they’re easiest to treat. And here’s the optimistic part: with vaccination, we can slash the risk dramatically. Studies show HPV vaccines prevent up to 90% of these cancers.
Factors like smoking or a weakened immune system can increase risks, but lifestyle choices help mitigate them. Think of it this way: knowledge about the hpv virus turns a potential threat into something we can control. Many who get diagnosed early go on to live full, healthy lives, proving that hope is always on the horizon.
Preventing Infection from HPV Virus
Prevention is the name of the game when it comes to the hpv virus, and luckily, there are several effective strategies. First off, vaccination stands out as the superstar – getting the shot before exposure can protect against the most harmful types. Safe sex practices, like using condoms consistently, cut down transmission risks, though they’re not foolproof.
Limiting sexual partners and getting regular check-ups also play key roles. For women, cervical screenings starting at age 21 can detect changes early. Men benefit from routine exams too, especially if they notice warts. Abstinence is 100% effective, but for those active, open communication with partners fosters mutual protection.
Education in schools and communities spreads awareness, reducing infections overall. It’s heartening to see global efforts, like WHO’s push for vaccination, making a dent in hpv virus rates. By adopting these habits, we’re not just protecting ourselves but building a healthier future. The hpv virus doesn’t have to win – we’ve got the tools to outsmart it.
The Role of the HPV Vaccine
Speaking of tools, the HPV vaccine is a breakthrough that’s changing lives. Vaccines like Gardasil 9 target nine high-risk types, including those causing most cancers and warts. Recommended for preteens around ages 11-12, it’s also available up to age 45 for catch-up.
The vaccine works by prompting your body to produce antibodies that fight the hpv virus before it takes hold. It’s given in two or three doses, depending on age – simpler than it sounds!

This schedule chart illustrates how easy it is to complete the series. Side effects are mild, like soreness at the injection site, and the benefits far outweigh any temporary discomfort. Millions have been vaccinated safely, leading to drops in infection rates worldwide. It’s optimistic stuff – imagine a world with fewer cancers thanks to this simple shot. If you’re eligible, talk to your doctor; it’s a step toward safeguarding against the hpv virus.
Diagnosis and Treatment Options for HPV Virus
Diagnosing the hpv virus often starts with visual checks for warts or screenings for abnormal cells. For women, a Pap smear combined with HPV testing is standard, while men might undergo anal Pap tests if at risk. Biopsies confirm suspicious areas.
Treatment varies: warts can be frozen, burned, or removed with creams like imiquimod. For precancerous changes, procedures like LEEP (loop electrosurgical excision procedure) remove affected tissue safely. No cure exists for the virus itself, but the body often clears it.
The positive spin? Advances mean treatments are less invasive and more effective. Follow-up care ensures everything’s under control, and many people move on without issues. Staying proactive with the hpv virus diagnosis leads to better outcomes – it’s all about catching it early.
- Topical treatments: For warts, options like podophyllin work wonders.
- Surgical removal: Quick and effective for stubborn growths.
- Monitoring: Regular check-ins for high-risk cases prevent escalation.
With these options, managing the hpv virus becomes straightforward.
Living Positively with HPV Virus
If you’ve got the hpv virus, take heart – millions live full lives with it. Focus on health: eat well, exercise, and avoid smoking to boost your immune system. Emotional support matters too; talking to friends or counselors eases any anxiety.
Relationships can thrive with honesty – disclose your status and use protection. Many find that the hpv virus doesn’t define them; it’s just a blip. Support groups online offer camaraderie, reminding you you’re not alone.
Optimistically, research continues, promising even better managements. Embrace self-care routines, like yoga or mindfulness, to stay balanced. Life with the hpv virus can be vibrant – it’s about perspective and proactive steps.
Debunking Myths About HPV Virus
Myths abound with the hpv virus, but let’s set the record straight. Myth one: Only promiscuous people get it. Nope – even one partner can transmit it. Myth two: It always causes cancer. False; most infections are harmless.
Another: Men can’t get tested. Actually, while no routine test exists for men, symptom checks help. And no, the vaccine isn’t just for girls – it’s for everyone. Busting these clears up confusion, promoting better health decisions.
- Myth: HPV is rare. Fact: It’s the most common STI.
- Myth: Warts mean cancer. Fact: Different types cause each.
- Myth: Once you have it, you’re doomed. Fact: Most clear it naturally.
By debunking, we empower against the hpv virus.
Fazit
In wrapping up, the hpv virus might seem daunting at first glance, but with knowledge, prevention, and early action, it’s highly manageable. We’ve covered its nature, spread, symptoms, types, cancer links, prevention, vaccines, diagnosis, living tips, and myths – all pointing to a brighter outlook. Remember, vaccines and screenings are our best allies, turning potential risks into non-issues. Stay informed, get vaccinated if you can, and encourage others to do the same. The future looks promising as we continue to combat the hpv virus effectively.
FAQs
What is the hpv virus?
The hpv virus is a common group of viruses that can cause warts or, in rare cases, lead to certain cancers, but most infections resolve on their own.
How can I prevent the hpv virus?
Prevent the hpv virus through vaccination, safe sex practices like using condoms, and regular health screenings.
Does the hpv virus always cause symptoms?
No, the hpv virus often shows no symptoms, which is why regular check-ups are important.
Is there a cure for the hpv virus?
There’s no cure for the hpv virus itself, but treatments manage symptoms and related conditions effectively.
Who should get the HPV vaccine?
The HPV vaccine is recommended for preteens, but catch-up shots are available up to age 45 to protect against the hpv virus.